Hospice care is a compassionate form of care designed for individuals facing the end of life. It focuses on comfort and quality of life rather than curative treatment. Understanding how to qualify for hospice care is essential for patients and their families as they navigate the final stages of a terminal illness.
Qualifying for Hospice Care
The process of qualifying for hospice care involves meeting specific medical criteria and making important decisions regarding end-of-life care preferences. Here are the steps and requirements for qualifying for hospice care:
1. Diagnosis of a Terminal Illness: To qualify for hospice care, an individual must be diagnosed with a terminal illness with a prognosis of six months or less to live if the disease follows its usual course. This diagnosis must be certified by a physician.
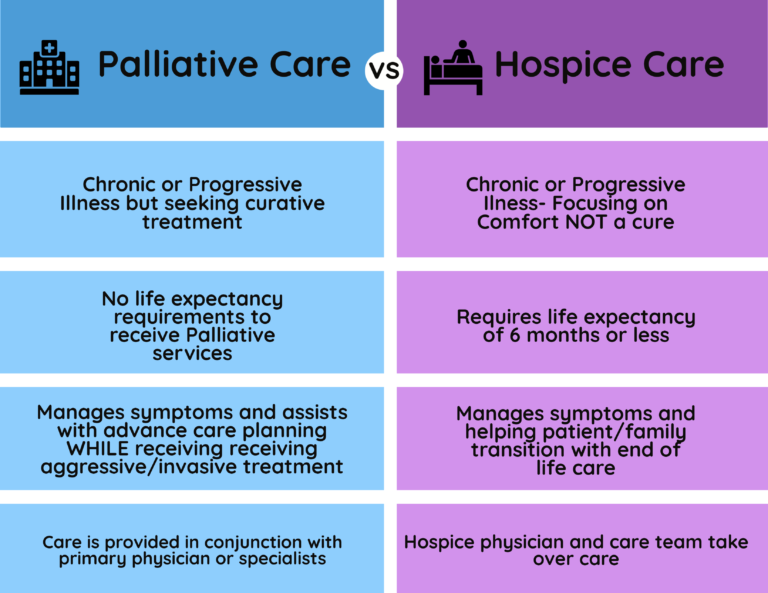
2. Acceptance of Palliative Care: The patient must choose to receive palliative care, which focuses on managing symptoms and providing comfort, rather than seeking curative treatments for their illness. This decision is often made after considering the patient’s values, goals for care, and the potential benefits and burdens of continued curative treatments.
3. Physician Certification: The patient’s attending physician and the hospice medical director must both certify that the patient is terminally ill and meets the hospice eligibility criteria. This certification is part of the required documentation for hospice care services.
4. Creation of a Care Plan: Once eligibility is established, the hospice team works with the patient and their family to create a personalized care plan that addresses the patient’s medical, emotional, and spiritual needs. This plan guides the hospice care provided.
5. Medicare or Insurance Coverage: Most patients use Medicare’s Hospice Benefit to cover hospice care services. Private insurance and Medicaid also often cover hospice care. It’s important to verify coverage and understand any potential out-of-pocket costs before beginning hospice services.
6. Choosing a Hospice Provider: Patients and families should select a Medicare-approved hospice provider that aligns with their needs and preferences. In the Bronx, Medflyt provides a selection of licensed caregivers who offer a range of hospice care services, including personal care assistance, medication management, and respite care for families.

The eligibility requirements for hospice care, as outlined in the provided sources, include the following key criteria:
- Terminal Illness Diagnosis: The patient must be diagnosed with a terminal illness, with a prognosis of six months or less to live if the illness runs its normal course.
- Physician Certification: At least two physicians, typically the patient’s attending physician and the hospice medical director, must certify that the patient is terminally ill. This certification is part of the required documentation for hospice care services.
- Acceptance of Palliative Care: The patient must choose palliative care, which focuses on comfort and symptom management, rather than curative treatments for their illness. This decision involves signing a statement choosing hospice care instead of other Medicare-covered treatments for the terminal illness.
- Medicare Part A Coverage: To elect hospice under Medicare, the individual must be entitled to Medicare Part A.
- Assessment Tools: Tools such as the Palliative Performance Scale (PPS), Karnofsky Performance Status Scale, or the Functional Assessment Staging (FAST) Scale may be used to assess a patient’s condition and determine eligibility for hospice care.
- Disease-Specific Criteria: Certain conditions may have specific criteria for hospice eligibility. For example, cancer patients may qualify if they have a decline in condition despite therapy, metastatic cancer, and a Palliative Performance Score of 70% or less. Dementia patients may be eligible when they have significant cognitive decline and other complicating factors such as difficulty swallowing or recurrent infections.
- Frequent Hospitalizations: A history of frequent hospitalizations or emergency room visits in the past six months can indicate that the disease has progressed to its end stages, suggesting that hospice care may be appropriate.
- Weight Loss and Decline: Progressive weight loss and a decline in conditions such as increased weakness, fatigue, and reduced functional abilities can be indicators for hospice eligibility.
- Informed Consent: The patient, or their legal representative if the patient is unable to make decisions, must be informed of the hospice philosophy and agree to receive hospice care services.
Hospice care covers a comprehensive range of services aimed at providing comfort and support to terminally ill patients and their families. According to the sources provided, the services covered by hospice care typically include:
- Doctor Services: Medical care provided by physicians who work with the hospice team to manage the patient’s care plan and address medical needs related to the terminal illness.
- Nursing Care: Registered nurses monitor the patient’s condition, administer medications, and provide medical care to manage symptoms and maintain comfort.
- Medical Equipment: Items such as hospital beds, wheelchairs, or walkers that are necessary for patient care at home.
- Medical Supplies: Supplies like bandages and catheters needed for the care of the patient.
- Drugs for Symptom Control and Pain Relief: Medications required to manage pain and other symptoms associated with the terminal illness.
- Home Health Aide and Homemaker Services: Assistance with personal care needs, such as bathing and dressing, as well as help with household tasks to maintain a safe and clean living environment.
- Physical and Occupational Therapy: Therapies to help maintain mobility and function, as well as assist with adapting to physical limitations.
- Speech Therapy: Services to help with problems such as swallowing, which can be an issue for some terminally ill patients.
- Social Worker Services: Support and counseling for the patient and family, assistance with practical and financial concerns, and help in accessing community resources.
- Dietary Counseling: Guidance on nutrition and dietary needs to ensure the patient’s nutritional requirements are met.
- Emotional and Spiritual Counseling: Support to help the patient and family cope with emotional and spiritual issues related to end-of-life and grief.
- Short-Term Inpatient Care: Care provided in a hospital or hospice facility for symptom management that cannot be handled at home, or to provide respite for family caregivers.
- Bereavement Support: Grief counseling and support services for the patient’s family following the death of the patient.
It’s important to note that while hospice care covers services related to the terminal illness, it does not include curative treatment for that illness, emergency department care not related to the terminal diagnosis, or room and board costs in a facility. The Medicare Hospice Benefit, Medicaid, and most private insurance plans typically cover these hospice services.
Conclusion
Qualifying for hospice care is a process that involves meeting medical eligibility requirements, making informed decisions about care preferences, and coordinating with healthcare providers. Hospice care offers a way for patients to spend their final months with dignity, surrounded by the comfort of their home and loved ones, while receiving compassionate care tailored to their needs. For residents of the Bronx, Medflyt provides access to quality hospice care services, ensuring that patients and their families receive the support they need during this challenging time.


